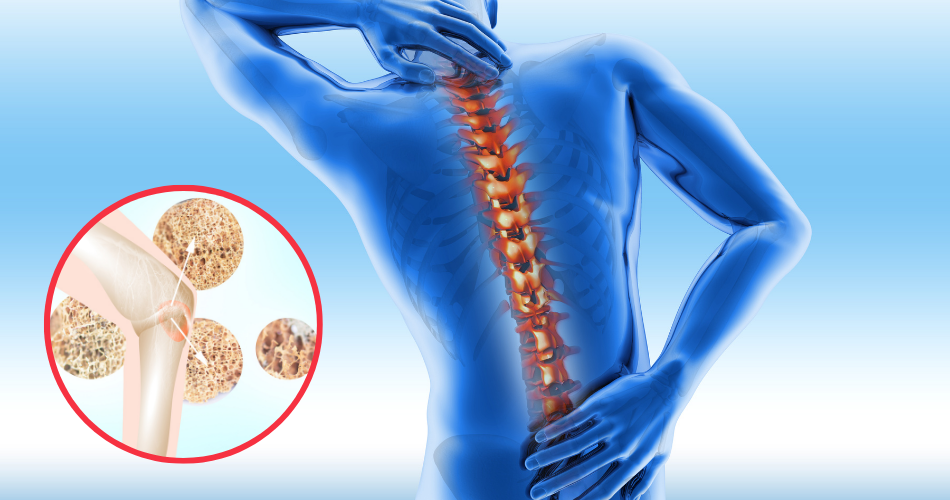
Osteoporosis is a medical anomaly in which bones become weak, increasing the risk of osteoporotic fractures. As a result, there is a decrease in the density of the bones, and bones get fractured by mild stress(1). Osteoporotic fractures occur primarily at the hip, wrist, or vertebral column.
Bones are the living tissue of the body that are remodeled constantly. The old bone matrix is removed, and the new matrix is deposited to maintain the strength of the bone.
Osteoporosis occurs when the rate of bone deposition doesn’t keep pace with the rate of bone removal. As a result, there is a decrease in bone density, and osteoporotic fractures occur.
Osteoporosis affects both sexes across the globe. However, women are affected more than men, especially postmenopausal women whose estrogen levels are decreased.
Unlike our skin, we can’t see our bones. Radiographic techniques are used to access bone health. However, some warning signs hint toward osteoporosis that shouldn’t be ignored.
Following are the 9 warning Osteoporosis symptoms to watch for:
1. Receding gums

Receding gums is one of the warning signs of osteoporosis. So if you have receding gums and bone pain, you shouldn’t take it lightly.
Many factors are responsible for receding gums, but osteoporotic bone loss is the most prominent.
Teeth are anchored in the jaw bone. If there is a decrease in the density of jaw bone, gums recede, pointing towards osteoporosis.
2. Loss of grip strength

As osteoporosis progresses, grip strength is significantly reduced. It is because there is decreased bone density and bone strength. As a result, efficiency and strength at the wrist joint are significantly depressed.
It happens mostly in postmenopausal women at old age. So there is already a risk of falling in old age that requires sound gripping and muscle strength.
However, as the grip strength declines, the risk of falling multiplies, leading to osteoporotic fractures.
3. Bone pain

As bone density is decreased in osteoporosis, bone aches when weight is put on it. Bone mass is significantly decreased, and the weight-bearing ability of the bones is depressed dramatically in the late stages of osteoporosis.
However, osteoporosis is not only the reason behind bone pain. Other conditions can also cause bone pain, such as osteomyelitis, bone infection, leukemia, mineral deficiencies, bone tumors, etc.
4. Muscle cramps

Muscle cramps are also observed if osteoporosis is associated with vitamin D deficiency. But, again, it’s because electrolytes distribution in the body becomes abnormal, leading to muscle pain and cramps.
5. Bone fractures

The most debilitating condition associated with osteoporosis is the frequent bone fractures(2). As the bones become brittle and less dense, the possibility of fractures is increased dramatically.
Osteoporotic fractures are observed in both sexes but more commonly in human females after menopause as the developing effect of estrogen on the bones is lost.
In the late stages of osteoporosis, minor traumas from falling or hitting an object can cause a bone fracture.
6. Height loss

Osteoporosis also induces changes in your physical appearance. For example, your height may get reduced. If you notice a more than 2 inches decrease in your height, you are in the risk zone of osteoporosis.
A decrease in height occurs because osteoporosis also affects your vertebrae and causes bending of the spine.
The more bending, the more reduction in height is noticed. A decrease in height is the warning sign that your condition has progressed to an advanced stage and should not be ignored at any cost.
7. Brittle fingernails

The health of your nails depicts the health of your bones. If your bones become weak and less dense, nails also become brittle and crack easily. However, it’s not always osteoporosis.
Many conditions can affect the nails, such as hypothyroidism, Raynaud’s syndrome, specific nutritional deficiencies, etc.
8. Altered posture

Osteoporosis produces an alteration in the posture. For example, the spine bends result in a condition known as kyphosis.
As vertebrae density decreases, there may be additional pressure on the airways and lungs, affecting breathing.
9. Osteoporosis and pain in the lower back

Osteoporosis also causes pain in the lower back. In addition, it can cause compression fractures of the vertebrae, which are extremely painful because the fractured vertebrae irritate the spinal nerves.
It causes shooting pain due to nerve root compression. Pain may vary in intensity from person to person.
If multiple vertebrae get fractured, the patient attains a stooped posture with a significant reduction in mobility.
Discover how to fix “Low Back” pain (INSTANTLY!)… 14,527+ Use Relaxing Movement Daily To Improve Posture and Reduce Back Pain.
Risk factors of osteoporosis
Following are the main factors that increase the risk of developing osteoporosis(3).
1. Age
Increasing age is one of the dominant causes of osteoporosis(4). It is because your bones are in a continuous state of remodeling. Normally, the rates of bone deposition and bone resorption are equal.
However, as a person grows old, an imbalance arises between bone deposition and resorption, which causes the bones to become fragile.
2. Menopause
In females, hormonal levels alter during their periodic cycles. Estrogen is one of the principal hormones which regulate bone development.
In old age, the monthly cycles of human females stop, known as a condition called menopause. At this stage, estrogen level declines leading to osteoporosis(5).
Men also experience similar effects due to a decrease in testosterone levels with age. However, the effect of decreased testosterone is less pronounced than estrogen.
3. Surgical removal of ovaries
If a human female’s ovaries are surgically removed due to some issues, the risk of developing osteoporosis multiplies due to altered hormonal levels.
4. Ethnicity
The risk of osteoporosis varies in different ethnic groups. For example, although it affects all races, the risk is comparatively greater in European and Asian women.
5. Hereditary
Positive family history also plays a role in osteoporosis. For example, if your parents or grandparents experienced osteoporotic fractures, you are more likely to develop the disease. About 30 genes are found to be associated with the development of osteoporosis.
6. Lifestyle
Exercise and physical work promote bone growth and development. Physical workload increases the strength of bones while staying sedentary weakens the bones increasing the risk of osteoporotic fractures.
7. Tobacco smoking
Tobacco smoking affects bone health. It weakens bones and decreases bone density. It also destroys the exogenous supply of estrogen, increasing the risk of developing osteoporosis.
8. Excessive alcoholism
Excessive alcoholism is quite damaging to health. It affects bones increasing the risk of osteoporotic fractures.
9. Malnutrition
Nutritional deficiencies can also lead to osteoporosis. The deficiency of minerals like calcium, phosphate, and magnesium is associated with decreased bone mass.
In addition, if someone has inadequate vitamin D in the body, bone mass decreases. Adequate dietary intake of proteins is also required in adolescence for proper bone growth. Protein deficiency is also linked to decreased bone mass.
10. Heavy metal poisoning
If you are exposed to heavy metals like lead or cadmium, you are more likely to develop osteoporosis.
Exposure to heavy metals causes a decrease in the density of bones in both sexes leading to osteoporotic fractures.
11. Immobilization
Mobilization and physical stress promote bone growth and development while sitting idle weakens bones. As a result, the bones of immobilized bedridden patients become extremely weak and prone to osteoporosis.
It is because the stress-induced bone growth is depressed. So, the bone resorption rate exceeds the bone formation rate weakening the bones and reducing the bones’ density.
12. Hypogonadism
Sex hormones affect bone growth. Testosterone and estrogen are the most crucial sex hormones involved in bone growth. Hypogonadal states like turner syndrome, hypothalamic amenorrhea, Klinefelter syndrome, etc., can lead to bone weakness and osteoporotic fractures.
Hemolytic disorders and osteoporosis:
Many hemolytic disorders affect bone health. Following hemolytic disorders can lead to osteoporosis and other effects on health and metabolism.
- Monoclonal gammopathies
- Multiple myeloma
- Leukemia
- Hemophilia
- Thalassemia
- Sickle cell disease
Genetic disorders and osteoporosis:
Many genetic disorders can also cause osteoporosis, such as:
- Marfan syndrome
- Osteogeneses imperfacta
- Hemochromatosis
- Multicentric Homocystinuria
- Menkes’ disease etc.
The bottom line:
Osteoporosis is a bone anomaly affecting both sexes with prevalence in females. It affects mainly older persons with a sedentary lifestyle. The risk is greater among postmenopausal women.
The causes and risk factors of osteoporosis are diverse. They are congenital and acquired and can also be grouped as lifestyle-related.
The warning signs of osteoporosis should not be taken lightly. Osteoporosis causes frequent bone fractures in old age, which is annoying and disabling.
Osteoporotic fractures should not be ignored, and proper medical assistance should be sought. In addition, taking care of your diet, avoiding a sedentary lifestyle, and adopting a healthy attitude help significantly reduce the risk of osteoporosis in old age(6).
References:
1. Lamichhane AP. Osteoporosis-an update. JNMA J Nepal Med Assoc. 2005 Jun;44(158):60–6.
2. Coughlan T, Dockery F. Osteoporosis and fracture risk in older people. Clin Med (Lond). 2014 Apr;14(2):187–91.
3. Lane NE. Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol. 2006 Feb;194(2 Suppl):S3-11.
4. Srivastava M, Deal C. Osteoporosis in elderly: prevention and treatment. Clin Geriatr Med. 2002 Aug;18(3):529–55.
5. Baccaro LF, Conde DM, Costa-Paiva L, Pinto-Neto AM. The epidemiology and management of postmenopausal osteoporosis: a viewpoint from Brazil. Clin Interv Aging. 2015;10:583–91.
6. Lane JM, Russell L, Khan SN. Osteoporosis. Clin Orthop Relat Res. 2000 Mar;(372):139–50.
7. Porter JL, Varacallo M. Osteoporosis. [Updated 2022 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441901/
8. InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Osteoporosis: Overview. 2008 Sep 11 [Updated 2018 Oct 18]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279529/

Sweet internet site, super design, real clean and utilise friendly.
Thank you! I’m glad you like my website 🙂
You could definitely see your enthusiasm in the work you write. The world hopes for more passionate writers like you who aren’t afraid to say how they believe. Always go after your heart.
Thank you so much!
Great line up. We will be linking to this great article on our site. Keep up the good writing.
Thank you!